TREATMENT Severe Acute Asthma
The primary goal is prevention of life-threatening asthma by early recognition of signs of deterioration and early intervention. As such, the principal goals of treatment include - Correction of significant hypoxemia
- Rapid reversal of airflow obstruction
- Reduction of the likelihood of recurrence of severe airflow obstruction
- Development of a written action plan in case of a further exacerbation
severity. The primary therapy of acute exacerbations is pharmacologic, which includes inhaled short-acting β2-agonists and, depending on the severity, systemic corticosteroids and O2 (Figs. 26–6 and 26–7). It is important that therapy not be delayed, so the initial history and physical examination should be obtained while initial therapy is being provided. Patients at risk for life-threatening exacerbations require special attention. Risk factors include a history of previous severe asthma exacerbations (e.g., hospitalizations, intubations, or hypoxic seizures), complicating illnesses (e.g., cardiac disease, diabetes, illicit drug use, or psychosis), use of more than two canisters per month of
short-acting inhaled β2-agonists, and current intake of oral corticosteroids or recent withdrawal from oral corticosteroids. A complete blood count may be appropriate for patients with fever or purulent sputum, but many patients will have a leukocytosis
from a viral infection or secondary to corticosteroid administration. Routine chest radiographs have not been shown to be of value unless physical findings suggestive of consolidations or pneumothoraces are present. Serum electrolytes should be monitored if highdose continuous inhaled or systemic β2-agonists are to be used because they can produce transient decreases in potassium, magnesium, and phosphate. The combination of high-dose β2-agonists and systemic corticosteroids occasionally may result in excessive elevations of glucose. Initial response should be achieved within minutes, and most patients experience significant improvement within the first 30 to 60 minutes of therapy, with most patients doubling their FEV1 or PEF.28 In patients ultimately admitted to the hospital, only a 10% to 20% predicted improvement is seen within the first 2 hours.Hypoxemia, primarily a result of ventilation-perfusion mismatch, is immediately correctable by low-flow oxygen. While reversal of lung function into the normal range may take 12 to 24 hours, complete restoration takes much longer—up to 3 to 7 days. A strategy to prevent recurrence such as systemic corticosteroids and PEF monitoring should be used. It is essential to provide the patient with a
self-management plan that includes a written action plan for dealing with exacerbations. Patients at risk for severe exacerbations should be taught how to use a peak-flow meter and monitor morning peak flows at home. In young children, an increased respiratory rate, increased heart rate, and inability to speak more than one or two words between breaths are signs of severe obstruction. Oxygen saturations by pulse oximetry and peak flows should be measured in all patients not
completely responding to initial intensive inhaled β2-agonist therapy.Initially, on admission, the peak flows or clinical symptoms should be monitored every 2 to 4 hours. Prior to discharge from the emergency department or hospital, the patient should be given a sufficient supply of prednisone, taught the purpose of the medications and proper inhaler technique, and given an appointment for a follow-up visit. Early recognition of deterioration and aggressive treatment are the keys to successful treatment of acute asthma exacerbations. Thus patient and/or parent education teaching self-management skills and written action plans for early institution of therapy for acute exacerbations
improve outcomes.7 For more moderate to severe patients, this therapeutic plan also may include the availability of oral prednisone to begin at home. Easy access by telephone to health care providers is also needed. Because of the rapid progression to severe asthma that can occur, patients and parents should be encouraged to communicate promptly with their asthma care provider during an exacerbation. Systemic corticosteroids and aggressive use of inhaled β2-agonists continue to be the cornerstones of therapy for acute severe asthma exacerbations. Figures 26–6 and 26–7 illustrate the recommended therapies for the treatment of acute asthma exacerbations in home and emergency department/hospital settings, respectively. The dosages of the drugs for acute severe asthma are provided in Table 26–6. Institutions should strongly consider developing critical-pathways/treatment algorithms for their emergency departments because their implementation
has been shown to improve outcomes and decrease the cost of care.
has been shown to improve outcomes and decrease the cost of care.
NONPHARMACOLOGIC THERAPY
Infants and young children may be mildly dehydrated owing to increased insensible loss, vomiting, and decreased intake. Unless dehydration has occurred, increased fluid therapy is not indicated in acute asthma management because the capillary leak from cytokines and increased negative intrathoracic pressures may promote edema in the airways. Correction of significant dehydration is always indicated, and the urine specific gravity may help to guide therapy in young children, in whom the state of hydration may be difficult to determine. Chest physical therapy and mucolytics are not indicated in the
Infants and young children may be mildly dehydrated owing to increased insensible loss, vomiting, and decreased intake. Unless dehydration has occurred, increased fluid therapy is not indicated in acute asthma management because the capillary leak from cytokines and increased negative intrathoracic pressures may promote edema in the airways. Correction of significant dehydration is always indicated, and the urine specific gravity may help to guide therapy in young children, in whom the state of hydration may be difficult to determine. Chest physical therapy and mucolytics are not indicated in the
therapy of acute asthma. Sedatives should not be given because anxiety may be a sign of hypoxemia, which could be worsened by central nervous system depressants. Antibiotics also are not indicated routinely because viral respiratory tract infections are the primary cause of asthma exacerbations. Antibiotics should be reserved for patients who have signs and symptoms of pneumonia (e.g., fever, pulmonary consolidation, and purulent sputum from polymorphonuclear leukocytes). Mycoplasma and Chlamydia are infrequent causes of severe asthma exacerbations but should be considered in patients with high oxygen requirements.espiratory failure or impending respiratory failure as measured
by rising PaCO2 (>45 mm Hg) or failure to correct hypoxemia with supplemental oxygen therapy is treated with intubation and mechanical ventilation. In order to prevent barotrauma and pneumothoraces from excess positive pressure, it is recommended that controlled hypoventilation or permissive hypercapnia be used (correcting the hypoxemia, PaO2 > 60 mm Hg, but allowing the PaCO2 to rise to the high 60 mm Hg range).
by rising PaCO2 (>45 mm Hg) or failure to correct hypoxemia with supplemental oxygen therapy is treated with intubation and mechanical ventilation. In order to prevent barotrauma and pneumothoraces from excess positive pressure, it is recommended that controlled hypoventilation or permissive hypercapnia be used (correcting the hypoxemia, PaO2 > 60 mm Hg, but allowing the PaCO2 to rise to the high 60 mm Hg range).
PHARMACOTHERAPY
β2-AGONISTS
The short-acting inhaled β2-agonists are the most effective bronchodilators and the treatment of first choice for the management of severe acute asthma. Up to 66% of adults presenting to an emergency department require only three doses of 2.5 mg nebulized albuterol to be discharged. Most well-controlled clinical trials have demonstrated equal to greater efficacy and greater safety of aerosolized β2-agonists over systemic administration regardless of the severity of obstruction. Systemic adverse effects, hypokalemia, hyperglycemia, tachycardia, and cardiac dysrhythmias are more pronounced in patients receiving systemic β2- agonist therapy. Children younger than 2 years of age achieve clinically significant responses from nebulized albuterol. Effective doses of aerosolized β2-agonists can be delivered successfully through mechanical ventilator circuits to infants, children,
and adults in respiratory failure secondary to severe airways obstruction. Frequent administration of inhaled β2-agonists (every 20 minutes or continuous nebulization) has been found to be superior to the same dosage administered at 1-hour intervals. In the subset of more severely obstructed patients, continuous nebulization decreases the hospital admission rate, provides greater improvement in the FEV1 and PEF, and reduces duration of hospitalization when compared with intermittent (hourly) nebulized albuterol in the same total dose. Thus continuous nebulization is recommended for patients having an unsatisfactory response (achieving less than 50% of normal FEV1 or PEF) following the initial three doses (every 20 minutes) of aerosolized β2-agonists and potentially for patients presenting initially with PEF or FEV1 values of less than 30% of predicted normal. The doses of inhaled β2-agonists for severe acute asthma (see Table 26–6) have been derived empirically. The β2-agonists follow a log-linear dose-response curve. In addition, the dose-response curve is shifted to the right by more severe bronchospasm or by increased concentrations of bronchospastic mediators, which is characteristic of functional antagonists. The ability to increase the dose of the short-acting aerosolized β2-agonists by as much as five- to tenfold over doses producing adequate bronchodilation in chronic stable asthmatics is what contributes to their efficacy in reversing the bronchospasm of acute severe asthma. The nebulizer dose of inhaled β2-agonists for children often is listed on a weight basis (milligrams per kilogram). However, a fixed minimal dose (2.5 mg albuterol or equivalent), as opposed to a weight-adjusted dose, is more appropriate in younger children because children younger than 5 years of age receive a lower lung dose. Adults dosed on a weight basis demonstrate excessive cardiac stimulation, so they have fixed maximal doses27 (see Table 26–6). Initial doses of inhaled β2-agonists can produce vasodilation, worsening ventilation-perfusion mismatch, slightly lowering oxygen saturation or Pao2. High-doses of inhaled β2-agonists can produce a decrease in serum potassium concentration, an increase in heart rate, and an increase in serum glucose concentration.
However, both children and adults receiving continuously nebulized β2-agonists have demonstrated decreased heart rates as their lung function improves. Thus an elevated heart rate is not an indication
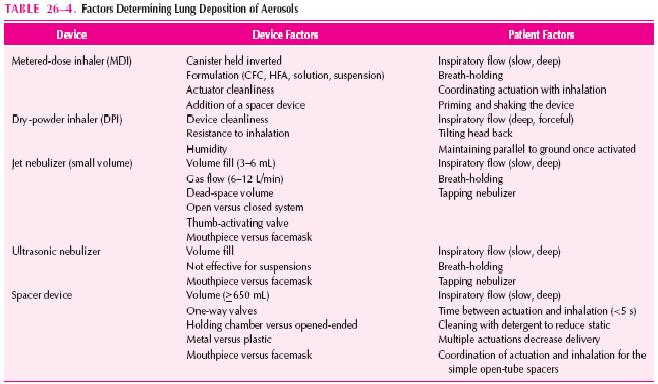
to use lower doses or to avoid using inhaled β2-agonists. Some controversy exists concerning the most cost-effective delivery system (MDI plus holding chamber versus nebulization) to be used in treating severe acute asthma in the emergency department and hospital (see below). The DPIs are currently not indicated for the treatment of severe acute asthma exacerbations. Patients with more severe obstruction may not be able to generate sufficient peak inspiratory flows for adequate delivery.
However, both children and adults receiving continuously nebulized β2-agonists have demonstrated decreased heart rates as their lung function improves. Thus an elevated heart rate is not an indication
to use lower doses or to avoid using inhaled β2-agonists. Some controversy exists concerning the most cost-effective delivery system (MDI plus holding chamber versus nebulization) to be used in treating severe acute asthma in the emergency department and hospital (see below). The DPIs are currently not indicated for the treatment of severe acute asthma exacerbations. Patients with more severe obstruction may not be able to generate sufficient peak inspiratory flows for adequate delivery.
CORTICOSTEROIDS
Systemic corticosteroids are indicated in all patients with acute severe asthma not responding completely to initial inhaled β2-agonist administration (every 20 minutes for three to four doses). Intravenous therapy offers no therapeutic advantage over oral administration.2This therapy usually is continued until hospital discharge. Tapering the dose in acute asthma following discharge from the hospital appears unnecessary, provided that patients are prescribed inhaled corticosteroids for outpatient therapy. Most patients achieve 70% of predicted normal FEV1 within 48 hours and 80% of predicted by 6 days after plateauing by day 3. Thus, maintaining systemic corticosteroid courses for 10 to 14 days may be unnecessarily long in some patients. Indeed, many patients not admitted to the hospital respond to 3- to 5-day courses of systemic corticosteroids. Short courses of oral prednisone (3 to 10 days) have been effective in preventing hospitalizations in infants and young children.2 It is recommended that a full dose of the corticosteroid be continued until the patient’s peak flow reaches 80% of predicted normal or personal best. Multiple daily dosing of systemic corticosteroids for the initial therapy of acute asthma exacerbations appears warranted because
receptor-binding affinities of lung corticosteroid receptors are decreased in the face of airway inflammation. However, patients with less severe exacerbations may be treated adequately with oncedaily administration. High-dose and very-high-pulse-dose corticosteroid regimens have not been shown to enhance the outcomes in severe acute asthma but are associated with a higher likelihood of
side effects. A recommended practice is to increase or double the dose of inhaled corticosteroids in patients who are experiencing a deterioration of their asthma control to prevent an exacerbation that requires emergency care. Studies of inhaled corticosteroids (ICSs) in acute exacerbations of asthma have provided conflicting results. Currently, there is insufficient evidence supporting efficacy in the emergency department setting. However, there is some evidence that prescribing ICSs on discharge from the emergency department reduces the risk of relapse. This policy seems like a reasonable recommendation because inflammation is the underlying cause of deterioration in most cases.
ANTICHOLINERGICS
Inhaled ipratropium bromide generally produces a further improvement in lung function of 10% to 15% over inhaled β2-agonists alone. In children and adults, multiple-dose ipratropium bromide added to initial therapy also produced a reduced hospitalization rate in the subset of patients with an FEV1 of less than 30% of predicted at baseline. Ipratropium bromide, a quaternary amine, is poorly absorbed and produces minimal or no systemic effects. Care should be used when administering ipratropium bromide by nebulizer. If a tight mask or mouthpiece is not used, the ipratropium bromide that deposits in the eyes may produce pupillary dilatation and difficulty in accommodation. Ipratropium bromide is not a vasodilator, so unlike β2-agonists it will not worsen ventilation-perfusion mismatc.
ALTERNATIVE THERAPIES
The emergency department use of aminophylline, a moderate bronchodilator,for acute asthma has not been recommended for a number of years. Clinical trials of aminophylline in adults and children hospitalized with acute asthma have not reported sufficient evidence of efficacy (improvement in lung function and reduced hospital stay) but have reported an increased risk of adverse effects. However, two studies of aminophylline in children with severe disease suggested a possible small benefit in reducing intensive care unit admissions. Adverse effects of theophylline include nausea and vomiting and potentiation of the cardiac effects of the inhaled β2-agonists. Magnesium sulfate is a moderately potent bronchodilator that is similar to aminophylline, producing relaxation of smooth muscle and central nervous system depression. The use of intravenous magnesium sulfate in patients presenting to the emergency department is controversial (see below). The adverse effects of magnesium sulfate include hypotension, facial flushing, sweating, nausea, loss of deep tendon reflexes, and respiratory depression. Patients have required dopamine to treat the hypotension.
Helium is an inert gas of low density with no pharmacologic properties that can lower resistance to gas flowand increase ventilation because the low density decreases the pressure gradient needed to achieve a given level of turbulent flow, converting turbulent flow to aminar flow. Helium is given as a mixture of helium and oxygen (heliox), usually 60% to 70% helium with 30% to 40% oxygen. As
with a number of experimental approaches, heliox was reported to be efficacious in initial nonrandomized clinical trials. However, the small number of randomized, controlled trials completed to date have failed to document efficacy. Although heliox is free of adverse effects, its use is limited to patients with a low inspired oxygen requirement because the decrease in density generally is insignificant clinically with less than 60% helium. The inhalational anesthetics halothane, isoflurane, and enflurane all have been reported to have a positive effect in children and adults with severe asthma that is unresponsive to standard medical therapy. The proposed mechanisms for inhalational anesthetics include direct action on bronchial smooth muscle, inhibition of airway reflexes, attenuation of histamine-induced bronchospasm, and interaction with β2-adrenergic receptors. well -controlled trials with these agents have not been completed. Potential adverse effects include myocardial depression, vasodilation, arrhythmias, and depression of mucociliary function. In addition, the practical problem of delivery and scavenging these agents in the intensive care environment as opposed to the operating room is a concern. The use of volatile anesthetics cannot be recommended based on insufficient evidence of efficacy.
Ketamine has been recommended for rapid induction of anesthesia in patients with asthma who require intubation and mechanical ventilation. Ketamine is thought to produce bronchodilation from
a combination of an increase in circulating catecholamines, direct smooth muscle relaxation, and inhibition of vagal flow. Anecdotal reports have suggested that ketamine is useful as a short-term adjunct in severe acute asthma; controlled trials have not provided sufficient evidence of efficacy, however. Ketamine has several significant adverse effects, including the anesthesia emergence reaction, which can alter mood and cause delirium. These emergence phenomena occur in at least 25% of patients over 16 years of age; the incidence seems to be much lower in younger patients. Other risks include an increase in heart rate, arterial blood pressure, and cerebral blood flow because
of its sympathetic effects.
SPECIAL POPULATIONS
6 Infants and children younger than 4 years of age may be at greater risk of respiratory failure than older children and adults. Although treated with the same drugs, these younger children require the use of a facemask as opposed to a mouthpiece for delivery of aerosolized medication. Use of the facemask reduces delivery of drug to the lung by one-half so that a minimal dose is recommended as
opposed to a weight-adjusted dose. The facemask should be sized appropriately and should fit snugly over the nose and mouth. Use of the “blow by” method, where the therapist or parent places the mask or extension tubing near the child’s nose and mouth, should be discouraged because holding the mask as few as 2 cm from the patient’s face reduces lung delivery of the aerosol by 80%.
Systemic corticosteroids are indicated in all patients with acute severe asthma not responding completely to initial inhaled β2-agonist administration (every 20 minutes for three to four doses). Intravenous therapy offers no therapeutic advantage over oral administration.2This therapy usually is continued until hospital discharge. Tapering the dose in acute asthma following discharge from the hospital appears unnecessary, provided that patients are prescribed inhaled corticosteroids for outpatient therapy. Most patients achieve 70% of predicted normal FEV1 within 48 hours and 80% of predicted by 6 days after plateauing by day 3. Thus, maintaining systemic corticosteroid courses for 10 to 14 days may be unnecessarily long in some patients. Indeed, many patients not admitted to the hospital respond to 3- to 5-day courses of systemic corticosteroids. Short courses of oral prednisone (3 to 10 days) have been effective in preventing hospitalizations in infants and young children.2 It is recommended that a full dose of the corticosteroid be continued until the patient’s peak flow reaches 80% of predicted normal or personal best. Multiple daily dosing of systemic corticosteroids for the initial therapy of acute asthma exacerbations appears warranted because
receptor-binding affinities of lung corticosteroid receptors are decreased in the face of airway inflammation. However, patients with less severe exacerbations may be treated adequately with oncedaily administration. High-dose and very-high-pulse-dose corticosteroid regimens have not been shown to enhance the outcomes in severe acute asthma but are associated with a higher likelihood of
side effects. A recommended practice is to increase or double the dose of inhaled corticosteroids in patients who are experiencing a deterioration of their asthma control to prevent an exacerbation that requires emergency care. Studies of inhaled corticosteroids (ICSs) in acute exacerbations of asthma have provided conflicting results. Currently, there is insufficient evidence supporting efficacy in the emergency department setting. However, there is some evidence that prescribing ICSs on discharge from the emergency department reduces the risk of relapse. This policy seems like a reasonable recommendation because inflammation is the underlying cause of deterioration in most cases.
ANTICHOLINERGICS
Inhaled ipratropium bromide generally produces a further improvement in lung function of 10% to 15% over inhaled β2-agonists alone. In children and adults, multiple-dose ipratropium bromide added to initial therapy also produced a reduced hospitalization rate in the subset of patients with an FEV1 of less than 30% of predicted at baseline. Ipratropium bromide, a quaternary amine, is poorly absorbed and produces minimal or no systemic effects. Care should be used when administering ipratropium bromide by nebulizer. If a tight mask or mouthpiece is not used, the ipratropium bromide that deposits in the eyes may produce pupillary dilatation and difficulty in accommodation. Ipratropium bromide is not a vasodilator, so unlike β2-agonists it will not worsen ventilation-perfusion mismatc.
ALTERNATIVE THERAPIES
The emergency department use of aminophylline, a moderate bronchodilator,for acute asthma has not been recommended for a number of years. Clinical trials of aminophylline in adults and children hospitalized with acute asthma have not reported sufficient evidence of efficacy (improvement in lung function and reduced hospital stay) but have reported an increased risk of adverse effects. However, two studies of aminophylline in children with severe disease suggested a possible small benefit in reducing intensive care unit admissions. Adverse effects of theophylline include nausea and vomiting and potentiation of the cardiac effects of the inhaled β2-agonists. Magnesium sulfate is a moderately potent bronchodilator that is similar to aminophylline, producing relaxation of smooth muscle and central nervous system depression. The use of intravenous magnesium sulfate in patients presenting to the emergency department is controversial (see below). The adverse effects of magnesium sulfate include hypotension, facial flushing, sweating, nausea, loss of deep tendon reflexes, and respiratory depression. Patients have required dopamine to treat the hypotension.
Helium is an inert gas of low density with no pharmacologic properties that can lower resistance to gas flowand increase ventilation because the low density decreases the pressure gradient needed to achieve a given level of turbulent flow, converting turbulent flow to aminar flow. Helium is given as a mixture of helium and oxygen (heliox), usually 60% to 70% helium with 30% to 40% oxygen. As
with a number of experimental approaches, heliox was reported to be efficacious in initial nonrandomized clinical trials. However, the small number of randomized, controlled trials completed to date have failed to document efficacy. Although heliox is free of adverse effects, its use is limited to patients with a low inspired oxygen requirement because the decrease in density generally is insignificant clinically with less than 60% helium. The inhalational anesthetics halothane, isoflurane, and enflurane all have been reported to have a positive effect in children and adults with severe asthma that is unresponsive to standard medical therapy. The proposed mechanisms for inhalational anesthetics include direct action on bronchial smooth muscle, inhibition of airway reflexes, attenuation of histamine-induced bronchospasm, and interaction with β2-adrenergic receptors. well -controlled trials with these agents have not been completed. Potential adverse effects include myocardial depression, vasodilation, arrhythmias, and depression of mucociliary function. In addition, the practical problem of delivery and scavenging these agents in the intensive care environment as opposed to the operating room is a concern. The use of volatile anesthetics cannot be recommended based on insufficient evidence of efficacy.
Ketamine has been recommended for rapid induction of anesthesia in patients with asthma who require intubation and mechanical ventilation. Ketamine is thought to produce bronchodilation from
a combination of an increase in circulating catecholamines, direct smooth muscle relaxation, and inhibition of vagal flow. Anecdotal reports have suggested that ketamine is useful as a short-term adjunct in severe acute asthma; controlled trials have not provided sufficient evidence of efficacy, however. Ketamine has several significant adverse effects, including the anesthesia emergence reaction, which can alter mood and cause delirium. These emergence phenomena occur in at least 25% of patients over 16 years of age; the incidence seems to be much lower in younger patients. Other risks include an increase in heart rate, arterial blood pressure, and cerebral blood flow because
of its sympathetic effects.
SPECIAL POPULATIONS
6 Infants and children younger than 4 years of age may be at greater risk of respiratory failure than older children and adults. Although treated with the same drugs, these younger children require the use of a facemask as opposed to a mouthpiece for delivery of aerosolized medication. Use of the facemask reduces delivery of drug to the lung by one-half so that a minimal dose is recommended as
opposed to a weight-adjusted dose. The facemask should be sized appropriately and should fit snugly over the nose and mouth. Use of the “blow by” method, where the therapist or parent places the mask or extension tubing near the child’s nose and mouth, should be discouraged because holding the mask as few as 2 cm from the patient’s face reduces lung delivery of the aerosol by 80%.